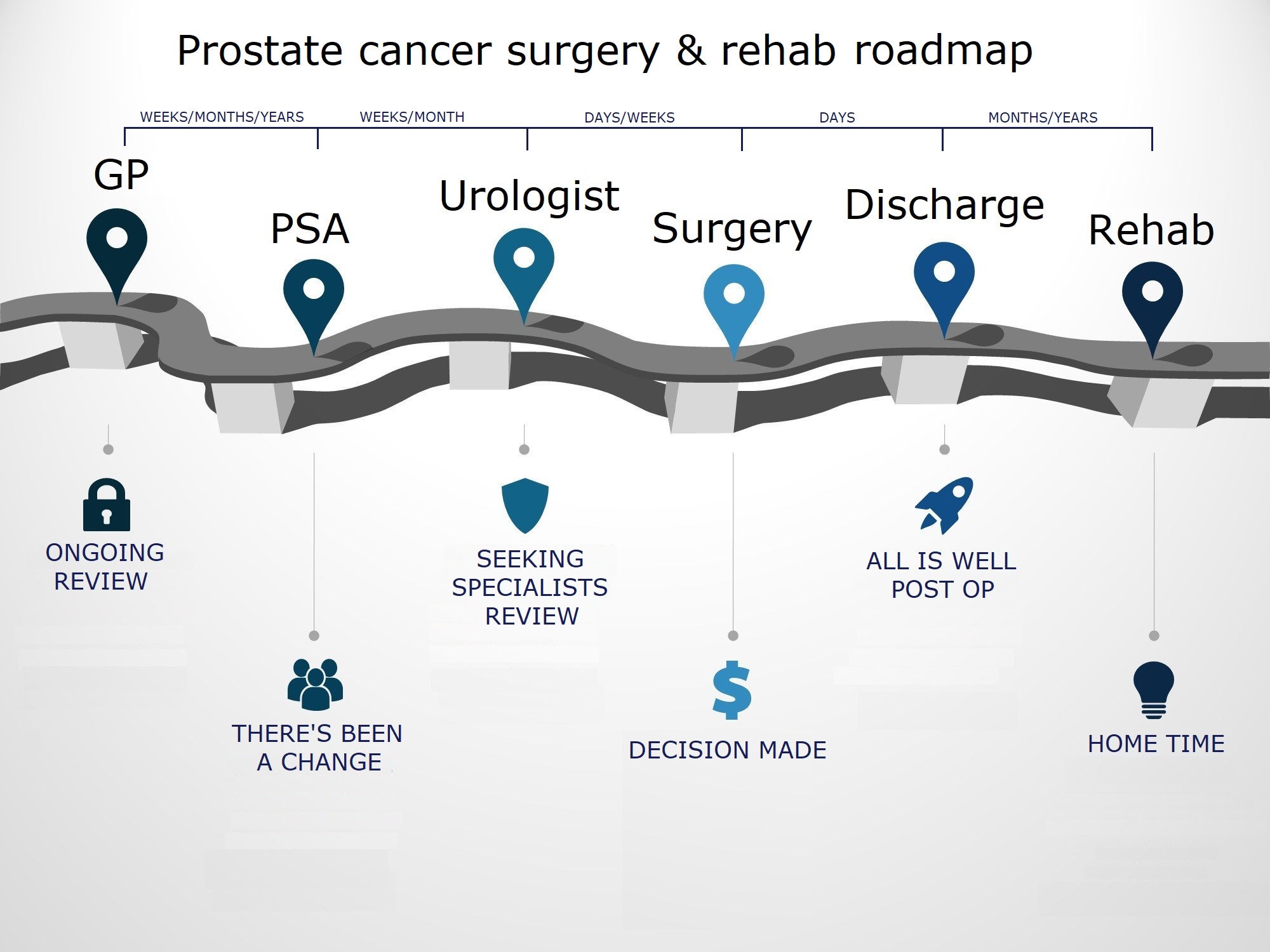
- In most circumstances a patient will be under review by their GP, either because they’ve been symptomatic (poor or reduced urine stream, getting up at night to urinate more than usual) or because they have a family history of prostate cancer. Your GP will typically review your blood pathology results (PSA test) and may perform a rectal prostate exam. In cases where PSA levels have increased more than your GP would consider normal, they will refer you to a Urologist for further examination. The relationship between changes in PSA level and prostate cancer is not linear. For example, a patient’s PSA level may increase from 2 to 5 and they may have prostate cancer whereas another patient’s PSA may increase from 15-18 and they may not have prostate cancer. This is why it is important to have a review with a Urologist
- Typically, when you see a Urologist, they will review your pathology, rectal exam and, if necessary, they may perform an ultrasound guided biopsy of the prostate. Your Urologist takes multiple cores to determine a Gleason Score (a system used to rank the aggressiveness of prostate cancer). Pending the result of the biopsy, your Urologist will opt for a either a “watch and wait” approach or advocate for a radical prostatectomy if the risks of leaving the prostate intact are outweighed by the possible progression of cancer beyond the prostate
- In the case of simple BPH (swelling of the prostate) your Urologist may prescribe medications such as tamsulosin, dutasteride or a combination to manage symptoms. Alternatively they may perform a Transurethral Resection of the Prostate (TURP). This surgery utilises a combined visual and surgical instrument called a resectoscope which is inserted through the tip of the penis and into the urethra. It acts like a re-bore or the prostate, relieving some of the pressure the prostate places on the urethra, allowing normal urine flow. It is worth noting that once you reach 50 years of age there is a 50% chance you will develop BPH, and for every year after your 50th birthday the percentage risk of developing BPH is the same as your age - i.e. at age 90 there is a 90% chance of developing BPH
- Once a diagnosis of prostate cancer is made and a radical prostatectomy is decided upon, patients are generally operated on within a small number of weeks. Da Vinci Robotic surgery is the gold standard for prostatectomy and involves having 5 small incisions made across your abdomen through which surgical instruments can be inserted. This technology is preferred because it is less traumatic, minimally invasive and enables the surgeon to overcome many of the shortcomings of both open prostatectomy (larger incision) and laparoscopic prostatectomy (smaller incision). The shortcomings of open prostatectomy and laparoscopic prostatectomy include reduced patient activity and mobility, increased time spent in hospital and more often results in loss of bladder control and sexual function because of damage to the delicate network of nerves around the prostate
- All forms of prostate surgery are quite expensive (approx $14,000-$20,000) and despite having private health insurance you will still encounter significant out of pocket expenses if the surgery is performed in the private setting (as opposed to having the surgery in the public system). Given the often urgent need for surgical intervention, many patients rely on the private health system to avoid the potential waiting lists of the public system
- Once the surgery is complete, your hospital stay is brief; with robotic prostatectomy your hospital stay is generally less than a week (it may even be one to two days). It is interesting to note that robotic surgery takes only 2-3 hours which is very quick compared to the other traditional removal options, hence some of the improved recovery times. It is also worth noting that all patients will have a catheter inserted for their surgery. The catheter usually remains in place for 7-10 days post-operatively, after which it is removed (assuming there hasn’t been any complications) by your Urologist or their registrar
- After this you will return home and begin your rehabilitation. This has historically involved a physiotherapist advising on pelvic floor exercises to correct incontinence but today we aim to treat more than continence
Research shows that vacuum therapy is a highly beneficial method of rehabilitation following radical prostatectomy.
The goal of penile rehabilitation therapy is to get good, regular blood flow into the penis. This aids in preventing atrophy and fibrosis (death of the cells/tissues and toughening of the blood vessels) of the penis. Beyond this you may find that regular use of the pump will also increase the length of the penis (noting a shortened penis length post-surgery) and maximise erectile function so that a spontaneous erection can be achieved in time.
The vacuum therapy device works by creating negative pressure around the penis, thereby increasing blood flow to the penis. When used as a treatment for erectile dysfunction (not for rehab post prostatectomy), the penile tube is placed over the penis, vacuum suction is applied and an erection is induced. Once the erection is achieved, a silicone constriction band is placed around the base of the penis and will hold the erection in place.
When using vacuum therapy for rehabilitation therapy post prostatectomy the pump is used in much the same way, except without the use of a constriction ring. Negative pressure is applied to increase blood flow to the penis, however, the constriction ring is not used because it prevents venous outflow and in fact reduces blood flow. Using vacuum therapy without the ring helps stimulate oxygenated blood flow, which can reduce the fibrotic changes that can occur after a radical prostatectomy. This is why vacuum therapy should be done daily for 10-15 minutes, ensuring that the penis is stretched out, limiting shortening and encouraging regular blood flow.
We feel that it is important you invest in a quality, medical-grade pump designed for therapeutic use. It’s important at this juncture not to buy a “toy” or “novelty” pump, but to look for a quality instrument, backed up by a solid reputation. Men’s Health Downunder have worked with Andromedical in the USA since 2015. We recommend their Pos-T-Vac device. It is TGA (Therapeutic Goods Administration) approved as a medical device in Australia, CE approved in Europe and FDA approved in the USA. It is widely recommended as the pump of choice by Urologists world wide and this is why we support them. It is available in the ‘Shop’ or via the link below.
Sample vacuum pump regimen
When using vacuum therapy for penile rehabilitation, the goal is to improve blood flow to the penis; this in turn helps to repair and maintain the penile tissue. A typical session involves the following steps:
- Apply the vacuum pump and draw blood into the penis (you may need to lightly shave around the base of the penis and use a little water based lubricant)
- Leave the penis fully engorged in the pump for 5 minutes
- Remove the pump and let the penis return to flaccid for 1 to 2 minutes
- Repeat the vacuum suction and hold the erection for another 5 minutes. This should be done 2-3 times. Alternatively you may wish to simply leave the pump over the penis for 10-15 minutes.
Doing this repeatedly can increase blood flow, decrease swelling, and increase lactate and oxygen exchange.
Rehabilitation tips
- Wait two full weeks after your catheter is removed before beginning rehabilitation
- Be patient, be patient and be persistent. It is common to not get full engorgement for some days or weeks
- Give yourself time to get familiar again with the sensation of being engorged. To do this, some men prefer to activate the pump for 30 seconds, and then rest for 30 seconds before activating the pump again. When starting your rehabilitation this ‘on/off’ process may be a gentle way to become acquainted with using the device
- The end point for use of the pump is generally after 6 months treatment which is when we start to see erectile function return
-

Step 1:
Attach the pump head to the penile tube. The pump head will look different depending on whether it’s with a manual or battery operated system.
-

Step 2:
Place the loading cone on the other end of the penile tube
-

Step 3:
Slide a tension ring over the top of the cone and down just past the base of the cone, on to the edge of the penile tube.
For your first time, we recommend using the tension ring size that’s in the middle. If the ring is too tight, you can move up to a larger size. And if your erection doesn’t last as long as you’d like, you can move down to a smaller size.
To slide the tension ring down to the base of the cone, place the middle ring over the top of the cone and use the two handles to move downward. Feel free to use lubricant if you need to.
-

Step 4:
Once the tension ring is securely on the penile tube, remove the cone.
-

Step 5:
Insert the bushing into the same end of the tube where you just removed the cone.
-

Step 6:
Apply lubricant to the bushing, the inside of the penile tube and the pubic area.
-

Step 7:
Place the lube-side end of the penile tube over your penis, being sure to hold the tube firmly to create a tight seal against your body.
-

Step 8:
Begin engaging the pump. For motor systems, you’ll press the red button. For manual systems, you’ll pull the handle. In both cases, the pump will begin drawing blood into your penis, forming an erection.
-

Step 9:
Once you’ve achieved the desired erection, slip the tension ring off the end of the penile tube and on to the base of your penis.
Step 10:
You now have a firm erection that will last for 30 minutes!
Your Urologist or Doctor may prescribe erection drugs which are injected into the penis. This is known as an intracavernosal injection (ICI). These medications are often used to bypass the oral route of administration. This can be for a number of reasons such as reducing side effects from oral medications, poor results from oral equivalents, drug interactions, impaired blood flow and so on. Despite the fact that injections can be uncomfortable (and certainly unnatural for most patients) they are very effective and with the correct dose and technique will be reliable.
Following a prostatectomy, the blood flow and nerve function to the penis are impaired and this causes a form of erectile dysfunction. This also explains why oral erection medications such as Viagra and Cialis do not work when taken as needed to achieve an erection - because the blood flow is impaired the medication cannot be delivered to the area where it is needed to elicit its effect. We use the analogy of the postman. Normal erectile function (pre-operatively), when blood flow to the penis is normal, is akin to the postman delivering your mail to your mailbox and you collecting the mail and replying to its contents on the same day. For example if you took Viagra or another similar erectile medication, blood flow will deliver the medication to the penis and its effect is seen. When blood flow to the penis and nerve function are impaired (post-operatively) it is like the postman jamming the mail into a full mailbox because the mail isn’t being collected. Therefore the content of the mail, in this case the medication taken orally, isn't received in a timely manner and therefore it isn’t replied to - the result is no erection. Using the same analogy, if we inject the medication into the penis, this is like having the mail delivered directly you, ensuring that the mail is replied to immediately. This is why ICI is always, where appropriate, recommended for patients post prostatectomy.
The 2 most commonly used medications for intracavernosal injection are Caverject (alprostadil) and Trimix, a mixture of 3 ingredients: alprostadil (PDE5i), phentolamine (alpha blocker), and papaverine (vasodilator). These ingredients work by relaxing the smooth muscle and opening the blood vessels in your penis, thus leading to an erection. An erection achieved with the use of ICIs is as close to natural as possible for a male post prostatectomy and sees a good amount of arterial blood flow into the penis. This ensures plenty of oxygen passes into the penis tissue, keeping it healthy. It also allows you to have intercourse or to masturbate, which is ideal for the rehabilitation of nerves. As with all the muscles in the body we adopt the phrase ‘use it or lose it’ and despite most patients initial hesitation to use ICI it is a very effective tool in the rehab bag of the Urologist, ensuring that the penis continues to be used in a time of otherwise inactivity.
Caverject is a propitiatory injection made by Pfizer which is available at most pharmacies (some may need to order it for you).
Trixmix comes in a range of strengths and is specially made by a sterile compounding Pharmacy. It needs to be specially compounded each time you need it. Men’s Health Downunder Pharmacists can arrange this for you. Please get in touch and we will be happy to arrange supply and ensure that you know how to use it safely and effectively.
Your Urologist/Doctor will decide which medication and dose is most appropriate for you and provide you with a prescription. It is generally recommended to be used weekly but this will depend on what instructions your doctor gives you. As for the duration of treatment with ICI, the end point is generally when erectile function starts to return (with or without the assistance of a higher dose PDE5i).
In patients post prostatectomy we use oral Phosphodiesterase 5 inhibitors (PDE5i) at low doses to increase blood flow to the penis. This will not likely result in an erection as the doses used tend to be lower than that required to aid sexual function. The other benefit inferred by low dose PDE5i is that they assist in keeping the blood vessel lining (the endothelial lining) healthy which is vital in getting oxygen from the blood into the penis tissue to keep it alive and functional. Generally a small dose of Viagra (sildenafil) or Cialis (tadalafil) might be used - 25mg Viagra or 5mg Cialis. The main benefit of tadalafil over sildenafil (or Levitra - vardenafil) is that it remains in the blood for a longer period of time, having an effect for more than 24 hours, whereas the others are only effective for 4-8 hours. This is important as we want to increase the blood flow to the penis 24 hours a day to get the maximum benefit. The drawback of tadalafil is its cost compared to sildenafil and this may need to be taken into consideration. Given the long half life of tadalafil it is still the PDE5i of choice and will ensure that the benefits of increased blood flow are achieved 24 hours a day, providing you with the best outcomes over the duration of treatment. Generally these medications are taken for a minimum of 6 months. Depending on the advice of your doctor and your progress, treatment may be longer.
- It is suggested that you begin rehabilitation 2-8 weeks post surgery. It is worth noting that 2 weeks post surgery, there will still be considerable inflammation and discomfort. For this reason it is suggested you wait until you are more comfortable or go very gently with any form of rehabilitation. Whilst it is never too late, it is always advisable to start rehabilitation as soon as possible; if you have any questions about timelines please feel free to contact our Men’s Health Downunder Pharmacists
- Most patients will have follow up PSA tests around 8 weeks post-operatively. At this stage PSA should be undetectable, given the prostate has been removed, unless the cancer has metastasised (spread) in which case PSA will be detected and you will need either a repeat PSA test and/or investigation for metastatic prostate cancer. When the prostate is removed the Urologist can check the margins of the prostate. If they are intact or described as in-situ you may be somewhat more optimistic; conversely if the margins are not intact you may have more reason for concern. Most patients will have this information given to them before being discharged postoperatively
- Having a PSA test after surgery can mean many things, so it is always best to talk to your Urologist about how the results relate to your individual case


