What is a Prostate?
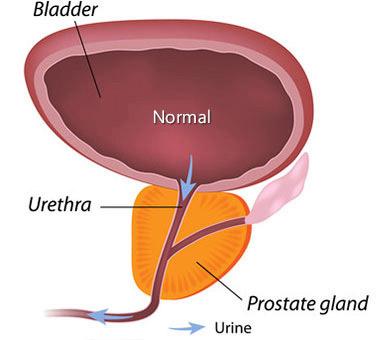
The prostate is a small gland that is part of the male reproductive system. It is usually about the size and shape of a walnut. Anatomically, the prostate rests below the bladder and in front of the rectum. The urethra passes through the prostate as it exits from the bladder. Physiologically the prostate and Cowper’s Gland, which adjoins the prostate, secrete fluid that nourish and protect sperm as they leave the testes during ejaculation. From here, the prostate squeezes this fluid into the urethra and it is expelled with sperm as semen.
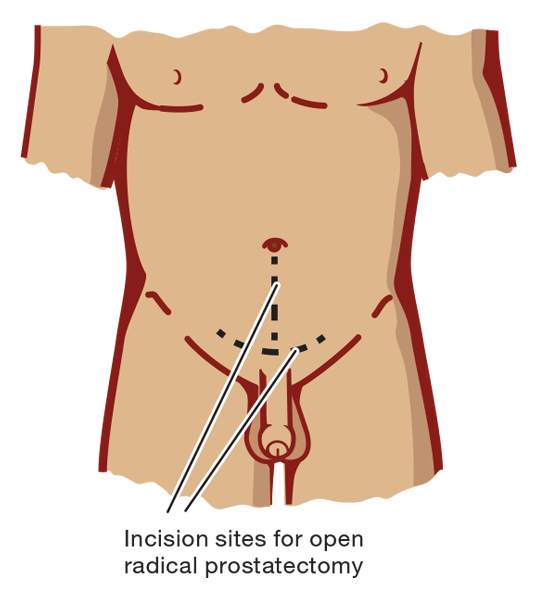
Open Radical Prostatectomy
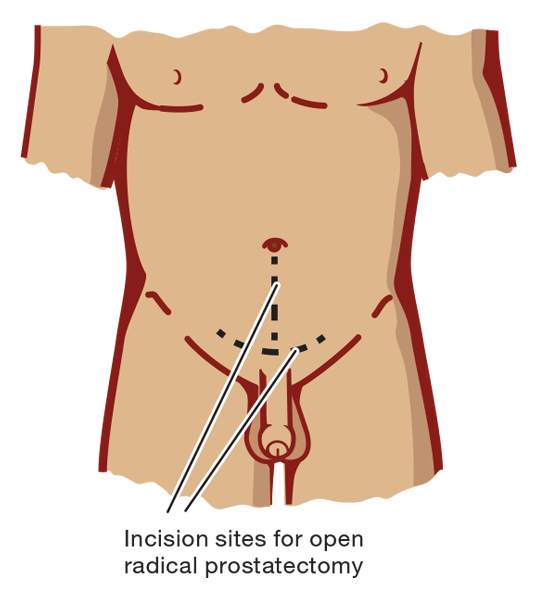
A radical prostatectomy consists of the removal of the entire prostate gland as well as some of the tissue around it, including the seminal vesicles. An open radical prostatectomy is the more traditional approach to the procedure, wherein the surgeon makes a single long incision to remove the prostate and nearby tissues. There are two main ways to perform this operation: radical retropubic prostatectomy and radical perineal prostatectomy. During a radical retropubic prostatectomy, an incision is made in the abdomen, from the belly button down to the pubic bone, while during a radical perineal prostatectomy, the incision is made between the anus and scrotum (the perineum). In either cases, the patient is asleep under general anesthesia or numbed with spinal or epidural anesthesia. The peritoneal approach is less common since it is more likely to cause erectile dysfunction, but it is also a shorter and faster procedure. During the retropubic approach, the surgeon may also remove some of the lymph nodes if they are affected by cancer.
RADICAL RETROPUBIC PROSTATECTOMY
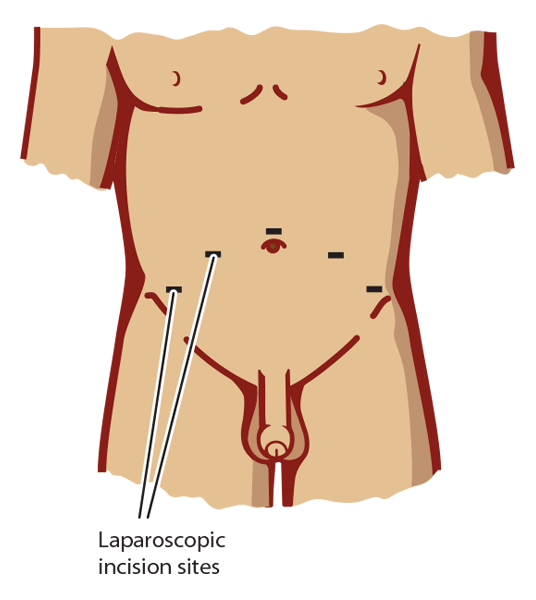
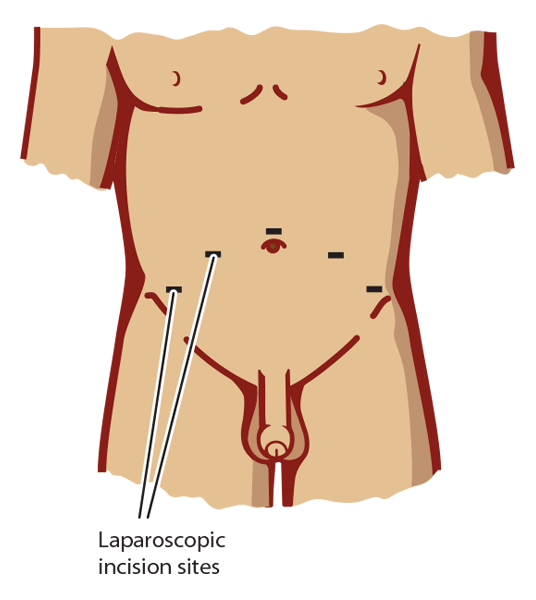
Laparoscopic Radical Prostatectomy
A laparoscopic radical prostatectomy is a more modern, less invasive and more likely nerve sparing form of prostatectomy that results in better post-operative outcomes with particular reference to erectile dysfunction, continence and general recovery. During a laparoscopic radical prostatectomy, the surgeon makes several small incisions and uses special long surgical tools to remove the prostate. When the surgeon holds the tools directly, the surgery is called laparoscopic radical prostatectomy. In addition to the surgical instruments, the surgeon also inserts a small camera called a laparoscope into the incision to increase visibility. This approach to prostatectomy has become more common, however today, surgeons will generally opt for robotic-assisted surgery where possible in the private system and where possible in the public system (the cost of purchasing the robot is often prohibitive for the public hospital system). In terms of ensuring the best possible post-operative outcomes, the most important factor of a laparoscopic radical prostatectomy is the skill and experience of your surgeon.
LAPAROSCOPIC RADICAL PROSTATECTOMY
Robotic-assisted Radical Prostatectomy
This is the latest and greatest option for men undergoing prostatectomy today. Robotic-assisted radical prostatectomy consists of the use a robotic interface called the da Vinci system to perform the operation. During a robotic-assisted laparoscopic radical prostatectomy, the surgeon sits at a control panel in the operating room where she or he control robotic arms which operate through several small incisions in the patient’s abdomen. For the surgeon, the robotic system provides greater manoeuvrability and more precision when moving the instruments than with standard laparoscopic radical prostatectomy. Generally this sees better postoperative outcomes with respect to erectile dysfunction, continence and general recovery. Still, it is worth noting that one of the most important factors in the success of either type of laparoscopic surgery is the surgeon’s experience and skill.
LAPAROSCOPIC RADICAL PROSTATECTOMY

Preoperative Expectation and Fears:
- While robotic prostatectomy is performed routinely, it is still a relatively major surgery that will take some time and effort to recover from. Life will be harder for at least a few weeks, if not months after surgery, however it is certainly preferable to the life-threatening hardships of letting the cancer progress unchecked. The underlying message to patients is to stay positive.
- What you can consider/do in preparation - our Preoperative Checklist
- Start pelvic floor exercises - it can be difficult to know if you’re performing them correctly so seek assistance if you are unsure
- Talk to other patients/support groups/doctor/pharmacist
- Start an oral PDE5i such as tadalafil - speak to your surgeon/doctor about this as early as possible as it may be worth starting before surgery
- Consider and optimise your blood pressure and diabetes control and where possible cease smoking, reduce alcohol intake and ensure your weight is within the healthy range - our Men’s Health Downunder pharmacists can help here
- One of the challenges of a prostate cancer diagnosis is that there is not a lot of time to prepare between a positive prostate biopsy result and scheduled surgery (this period can be as short as one to two weeks) meaning revision and discussion of items on the preoperative checklist should begin as early as possible
Risks and Benefits of Prostatectomy
The removal of the prostate via prostatectomy is known to be an effective method to treat prostate cancer, particularly in cases where the cancer is not believed to have metastasised. Laparoscopic prostatectomy (with or without robotic assistance) has some advantages over open radical prostatectomy, including less blood loss and pain, shorter hospital stays and faster recovery times (although the catheter will need to remain in the bladder for about the same amount of time). Similar to any other surgery, there are possible risks and side effects from having a prostatectomy. These risks include reactions to anaesthesia, bleeding from the surgery, blood clots in the legs or lungs, damage to nearby organs and infections at the site of surgery. These risks are less prevalent with laparoscopic surgery but are also influenced by the patient’s overall health and age, as well as the surgical team’s skills. Beyond surgery patients often experience side effects; the 2 most prevalent are urinary incontinence and erectile dysfunction.
Post-operative Expectations and Fears
There are a number of ‘big ticket’ outcomes patients want to see post prostatectomy. These include:
- Complete removal of an 'intact' prostate (cancer cells in-situ with clear margins)
- Recovery of continence
- Recovery of sexual function
- Preservation of penis length - if rehabilitation is not performed, atrophy and fibrosis of the penis can occur rendering it difficult to simply urinate (especially noting that post-operatively the penis immediately appears upward of 2.5cm shorter)
- Whilst the return of the the above are not guaranteed there are exercises and activities patients can undertake to ensure the best outcomes result
Beyond these patients can report the following concerns:
- Abdominal distention, constipation or bloating - ensure regularity with softeners such as coloxyl - no stimulant laxatives such as Sennakot or Coloxyl and Senna
- Bladder spasms - should resolve and are often secondary to urination
- Bloody drainage around the catheter or in the urine - can be a sign of not resting and will subside with rest. If it does not resolve with rest seek advice from your specialist
- Bruising around the port sites - not uncommon - will resolve with time. Hirudoid cream may help
- Lower leg and ankle swelling - not uncommon - will resolve with time. Try and elevate legs and wear compression stockings if needed
- Perineal discomfort - may last for several weeks post surgery. It may help to elevate the feet on a small stool when passing a bowel movement, apply haemorrhoid ointment (Proctosedyl), and increase the fibre and water intake in your diet
- Swelling and bruising of the penis and scrotum - not uncommon and is not a cause for serious concern. You might notice scrotal/penile swelling anywhere from immediately after surgery to five days post surgery. It should go away on its own in a week or two. It may help to elevate the scrotum on a small rolled up towel when sitting or lying down to reduce swelling. It is also advisable to wear supportive underwear (briefs, not boxer shorts) or employ the use of a medical scrotal support (available in the Mens Health Downunder store) if you are still experiencing problems.
Benign Prostate Hyperplasia (BPH)?
Benign prostatic hyperplasia (BPH) relates to enlargement of the prostate gland caused by a benign (non harmful) overgrowth of usually glandular prostate tissue. BPH usually presents as variable urine flow. This variable and often poor urinary flow is caused by constriction of the urethra and can be corrected by a procedure known as a TURP (Transurethral Resection of the Prostate).
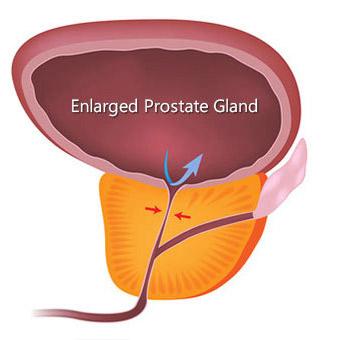
Typically BPH occurs in men over 50 years old, at which point the likelihood of a male having BPH is approximately 50%. The likelihood then increases by approximately 1% per year. I.e. at age 70 there is a 70% likelihood; at age 85 there is an 85% likelihood.
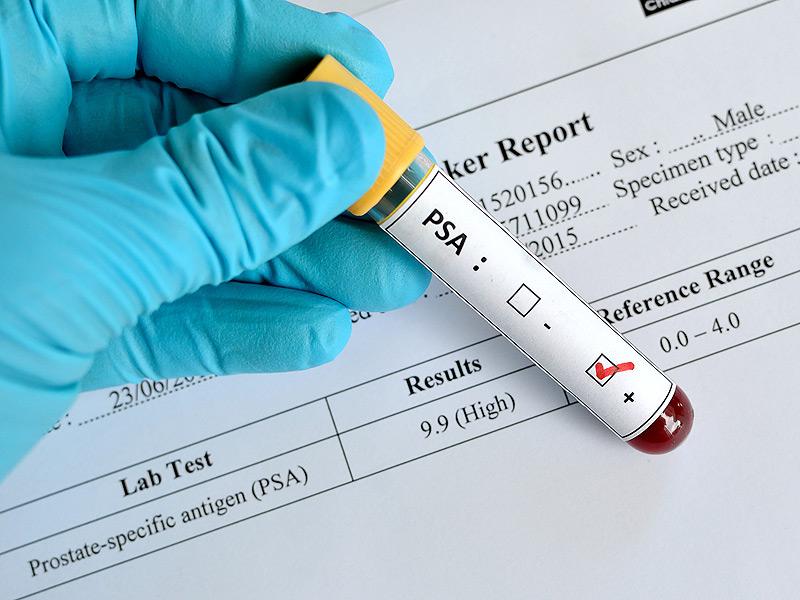
BPH is not a direct indicator of prostate cancer, however males experiencing BPH should speak to their GP about ongoing management strategies and pathology. All men over 50 should be having annual PSA blood tests and if deemed necessary rectal digital examination as for a number of men with active prostate cancer there will be no obvious signs or symptoms.
Prostate Specific Antigen (PSA)
PSA, or prostate specific antigen, is a protein produced only by prostate gland cells. Normally, men have low levels of PSA in their blood; we tend to find that the PSA level generally increases with age as the prostate enlarges (see BPH). It is worth noting however that PSA is not a specific test for prostate cancer, in much the same way that BPH does not necessarily indicate prostate cancer. It is however a marker of cancer risk. To confirm if cancer is present, it is necessary to take a biopsy of the prostate. The biopsy will also help to determine how aggressive a cancer is and in part will then guide the Urologist and patient on the appropriateness of prostatectomy. In essence PSA pathology is used in two ways: (1). To identify men at risk for prostate cancer before they develop symptoms (screening), and (2). To monitor men with prostate cancer. A single test is generally not used as the only indicator of prostate cancer risk. If the PSA is high, the test is usually repeated a few months later. The rate of change in the PSA level is a stronger indicator of prostate cancer risk; if the level doubles within a year it should be followed up by a Urologist.
You can first assess your general risk by using Risk Calculator 1 (no PSA result available) which takes into account your age, family history and urinary symptoms.
Once you know your PSA level, you can then use Risk Calculator 2 (using your PSA result). It will help you make a more informed decision about whether it would be wise to undergo further tests.
Transurethral Resection of the Prostate (TURP)
Transurethral resection of the prostate (TURP) is a surgery used to treat urinary problems due to an enlarged prostate. A combined visual and surgical instrument called a resectoscope is inserted through the tip of the penis and into the urethra, the tube that carries urine from your bladder. The prostate surrounds the urethra as shown in the below diagram.
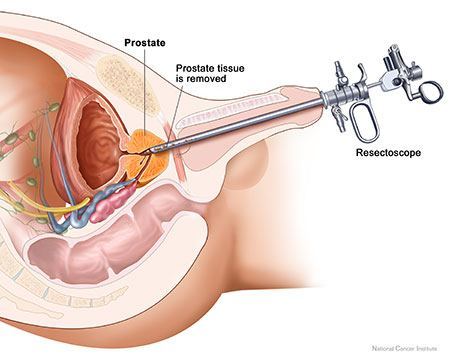
Using the resectoscope, the surgeon trims away the protruding prostate tissue that's blocking urine flow. TURP is generally considered an option for men with moderate to severe urinary problems that haven't responded to medication. Traditionally, TURP has been considered the most effective treatment for an enlarged prostate. However, a number of other, minimally invasive procedures are becoming more effective due to improved techniques and surgical tools. These minimally invasive procedures generally cause fewer complications and have a quicker recovery period than TURP.
Side effects of having had a TURP may include temporary difficulty urinating for a few days, urinary tract infection and blood in the urine.
It is likely your doctor will recommend that after a TURP you:
- Drink plenty of water to flush out the bladder
- Eat high-fibre foods to avoid constipation and straining during a bowel movement - taking a stool softener may also help
- Wait to resume taking any blood-thinning medications until given the ok by your doctor
- Avoid strenuous activity, such as heavy lifting, for four to six weeks or as advised
- Abstain from sex for four to six weeks
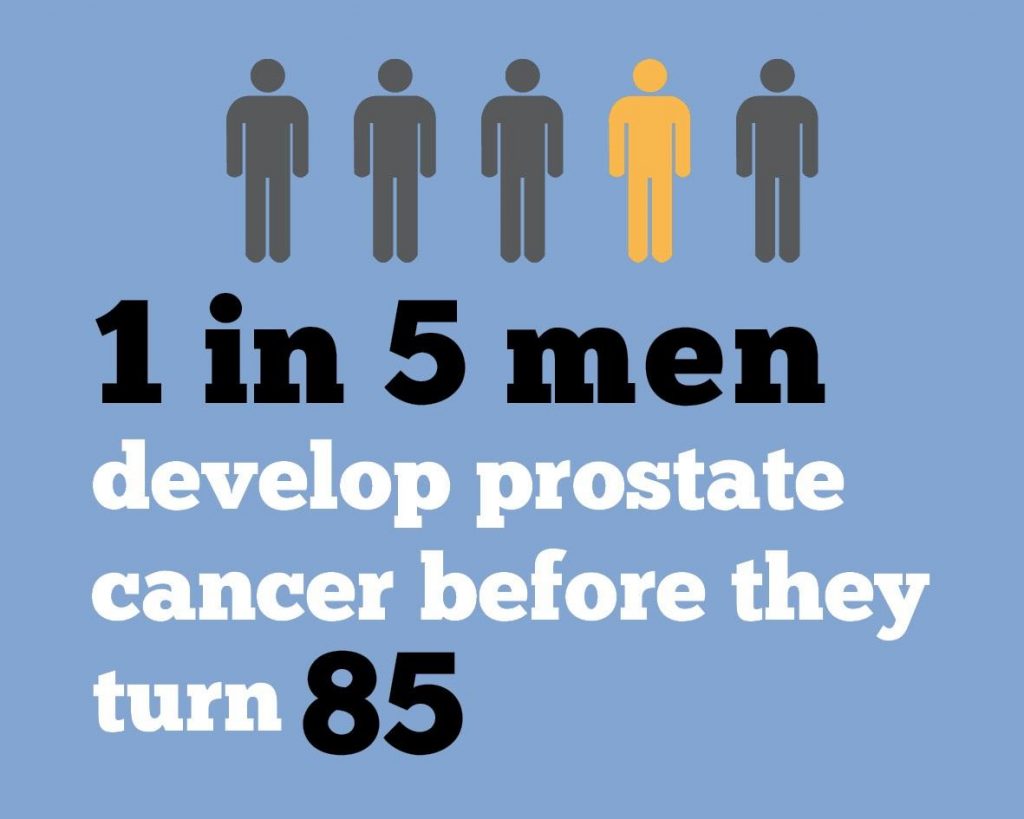
- An estimated 16,665 men were diagnosed with prostate cancer in 2017 (3rd to breast then bowel cancer)
- This accounted for 23.1% of all new cancer diagnoses in men
- An estimated 3452 men died of prostate cancer in 2017 (3rd behind lung and bowel)
- This accounted for 12.7% of all male cancer deaths
- The chance of 5 year survival was 95%
- At the end of 2012 there were 94,114 men living with prostate cancer who were diagnosed in the preceding 5 years
- The prostate is a small gland that is part of the male reproductive system. It is usually about the size and shape of a walnut. Anatomically the prostate rests below the bladder and in front of the rectum and the urethra passes through it as it exits from the bladder. Physiologically the prostate, and Cowper’s Gland which adjoins the prostate, secretes fluid that nourish and protect sperm AS THEY LEAVE the testes During ejaculation, the prostate squeezes this fluid into the urethra, and it’s expelled with sperm as semen.
a) Open radical prostatectomy
Open radical prostatectomy is an operation whereby an incision, approximately 10cm in length, is made in the lower abdomen (from below the belly button to the top of the pubic hair line or across the top of the pubic hair line).
OPEN RADICAL PROSTATECTOMY
b) Laparoscopic radical prostatectomy
Laparoscopic radical prostatectomy involves the urologist inserting a small camera and instruments (surgical tools) through several small incisions in your abdomen to look inside your body and perform the operation. Your abdomen is filled with carbon dioxide so the prostate and surrounding area can be clearly seen.
LAPAROSCOPIC RADICAL PROSTATECTOMY
c) Robotic assisted radical prostatectomy
Robotic-assisted radical prostatectomy is laparoscopic surgery performed with the assistance of equipment that helps with dexterity and 3-D vision. The surgeon performs the operation by controlling the surgical tools remotely with the aid of the computer. Small incisions in your abdomen are required. Robotic surgery isn’t available in all hospitals in Australia and currently can be financially costly.
d) Preoperative expectation/fears:
- While robotic prostatectomy is performed routinely, it is still a relatively major surgery that will take some time and effort to recover from. Life will be harder for at least a few weeks, if not months after surgery; however it is certainly preferable to the life-threatening hardships of letting the cancer progress unchecked. The underlying message for the patient is to stay positive.
- What you can consider/do in perperation
- Start pelvic floor exercises
- Talk to other patients/support groups/Doctor/Pharmacist
- Oral PDE5i such as Tadalafil
- Consider and optimise blood pressure and diabetes control and where possible cease smoking, reduce alcohol intake and ensure weight is within the healthy range
- Unfortunatey often there is not a lot of time to prepare between positive biopsy and surgery meaning postoperative attention should begin asap
e) Post-operative expectations/fears
There are a number of ‘big ticket’ outcomes patients want to see postoperatively. These include:
- Complete removal of an 'intack' prostate (cancer cells insitu with clear margins)
- Recovery of continence
- Recovery of sexual function
- Preservation of penis length; if no rehabilitation is performed atrophy of the penis can occur rendering it difficult to simply urinate (especially noting that postoperatively the penis appears upward of 2.5cm shorter immediately)
- whilst the return of the the above are not guaranteed there are exercises/activities patients can undertake to ensure best outcomes result
Beyond these patients can report the following concerns:
- Abdominal distention, constipation or bloating - ensure regularity with softners such as coloxyl - no stimulant laxatives such as Sennakot or Coloxyl and Senna
- Bladder spasms - should resolve and are often secondary to urination
- Bloody drainage around the catheter or in the urine - can be a sign of not resting and will subside with rest. If it does not resolve with rest seek advice from specialist
- Bruising around the port sites - not uncommon - will resolve with time. Hirudoid cream may be an option
- Lower legs/ankle swelling - not uncommon - will resolve with time. Try and elevate legs and wear stockings if need be
- Perineal discomfort - may last for several weeks post surgery. It may help to elevate the feet on a small stool when passing a bowel movement, applying hemorrhoid ointment (Proctosedyl), and to increase the fiber and water intake in the patient’s diet
- Scrotal/penis swelling and bruising - not uncommon and is not a cause for serious concern. The patient might notice scrotal/penile swelling anywhere from immediately after surgery to 5 days later. It should go away on its own in a week or two. It may be worth elevating the scrotum on a small rolled up towel when sitting or lying down to reduce swelling. It is also advisable to wearing supportive underwear (briefs, not boxer shorts) or if still problematic employ the use of a medical scrotal support
BPH
Benign prostatic hyperplasia (BPH) relates to enlargement of the prostate gland caused by a benign (non harmful) overgrowth of usually glandular prostate tissue which usually presents as variable urine flow. This variable, and often poor urinary flow, is caused by constriction of the urethra and can be corrected by having what is known as a TURP (transurethral resection of the prostate).
Typically BPH occurs in men over 50 years old; at which point the liklihood of a male having BPH is approximately 50%; the risk/liklihood increasing by 1%/year. Ie at age 70 there is a 70% liklihood; at age 85 there is an 85% likelihood.
BPH is not a direct indicator of prostate cancer, however males experiencing BPH should speak to their GP about management strageties and ensure that they have regular checkups incase of changes.
- Estimated 16665 males diagnosed in 2017 (3rd to breast then bowel cancer)
- This accounted for 23.1% of all new cancer diagnosis in males
- Estimated 3452 males died of prostate cancer in 2017 (3rd behind lung and bowel)
- This accounted for 12.7% of all male cancer deaths
- The chance of 5 year survival was 95%
- At the end of 2012 there were 94114 living with prostate cancer that were diagnosed in the preceeding 5 years


